Surgery of Sleep Apnea and Snoring Northridge, Westlake Village
What is Sleep Apnea?
Obstructive sleep apnea (OSA) is a syndrome characterized by periods of cessation of breathing (apnea) or decreases in airflow during sleep (hypopnea) that occur during sleep. The syndrome is defined by an apnea-hypopnea index (the number of apneas plus hypopneas divided by the number of hours asleep). The number is 5 or higher in association with excessive daytime sleepiness.
4 percent of men 30 to 60 years old, and 2 percent of women in this age group fit this criteria. Looking at larger studies, 24% of men have indexes greater than 5, and 9% of women have indexes greater than 5. The worse the syndrome, the higher the index, and in some cases the index can exceed 100. Risk factors for OSA include obesity, increased neck circumference, craniofacial abnormalities, hypothyroidism, and acromegaly.
Snoring is a symptom of sleep apnea, but not everyone who snores has the syndrome. Other disorders cause daytime sleepiness and include narcolepsy, periodic limb movement disorder, and circadian-rhythm abnormalities.
Clinically most people with sleep apnea snore loudly, grunt or struggle with breathing while sleeping, and this causes their bed partner to seek sleep in a different room. Partners will also note concern when they note long pauses in their bed partner’s patterns of breathing during sleep which is characteristic of sleep apnea. People with sleep apnea also have daytime sleepiness or somnolence, headaches, irritability, inability to concentrate, and fatigue. There are a number of medical conditions that are associated with OSA. Systemic hypertension or high blood pressure, and other cardiovascular diseases are associated with sleep apnea. Patients with sleep apnea have a three-fold increase in the rate of motor vehicle accidents. This rate falls to normal controls when those people are placed on CPAP.
The primary reason to be treated is to improve your quality of life. The risk factors associated with prolonged sleep apnea are known but not quantified. Clearly the risk of motor vehicle accidents is increased, but the true risk of sudden death, stroke, or heart attack because of sleep apnea is still unknown.
 |
Dr Kerner on Lifetime TVDr. Kerner on Lifetime TV’s “Speaking of Women’s Health” discussing women and snoring |
Diagnosis
People at risk for sleep apnea include those that are obese, hypertensive (high blood pressure), habitual snorers, and hypersomnolent (sleepy). We can predict the severity of OSA based on a combination of factors. Neck circumference or body-mass index correlates with severity. Neck circumference measurements are adapted by adding 4 cm for patients with high blood pressure, snoring ( 3 cm), or choking or gasping (3 cm). A low probability exists if the adjusted score is less than 43 cm, intermediate probability (4 to 8 times more likely) with a circumference between 43 and 48 cm, and a high probability (20 times) with an adjusted circumference greater than 48 cm. The Epworth Sleepiness Scale is a self administered questionnaire that helps determine how likely you are to fall asleep in certain situations.
| 0 = no chance of dozing |
| 1 = slight chance of dozing |
| 2 = moderate chance of dozing |
| 3 = high chance of dozing |
| SITUATION | CHANCE OF DOZING |
| Sitting and reading | ____________ |
| Watching TV | ____________ |
| Sitting inactive in a public place (e.g a theater or a meeting) | ____________ |
| As a passenger in a car for an hour without a break | ____________ |
| Lying down to rest in the afternoon when circumstances permit | ____________ |
| Sitting and talking to someone | ____________ |
| Sitting quietly after a lunch without alcohol | ____________ |
| In a car, while stopped for a few minutes in traffic | ____________ |
Polysomnography
Polysomnography or a sleep study is the gold standard for assessing patients for sleep apnea Northridge. A quality sleep lab is the best method for obtaining the appropriate data, however, some home studies can be effective. Home oximetry can be correlative, a test in which patients are monitored for desaturation which sleeping. The sleep study gives us considerable data that allows us to fully evaluate the quality of sleep, and with a CPAP (continuous positive airway pressure) titration study, we can determine what treatment parameters are required to reverse the apnea.
Treatment
Continuous positive airway pressure is the nonsurgical gold standard. CPAP clearly reverses the apnea, stops the snoring, improves quality of life and sleep, and increases alertness. The downside is only 50% of people can tolerate the machine for any length of time. There are considerable technical issues that have to be overcome including the fitting of the mask or nasal pillows, sleep positioning, and the issues associated with the bed partner.
For those people that have mild apnea or snoring, conservative therapy is initiated first. This includes weight loss, avoidance of benzodiazepines (sleeping pills or muscle relaxants), and the use of alcohol before bedtime. A 10% weight loss is associated with a 26% decrease in the apnea-hypopnea index.
Since weight loss takes time and is only marginally successful for most people, other treatments are available. Oral appliances have been designed for patients. These devices position the lower jaw, and therefore, modifies the airway. Long term studies with oral appliances are lacking in the medical literature, but they are clearly a suboptimal alternative to CPAP.
Surgical therapy is directed towards the different levels of airway obstruction that
occurs in sleep apnea. The airway from the nose to the larynx consists of the upper airway, and any place along this tract can have obstruction which may require correction. Additionally, the airway in sleep apnea must be reconstructed to both enlarge and tighten the tissues. Our approach is to first encourage patients to try CPAP. CPAP keeps the entire upper airway open using a positive pressure stream of air which opens the airway.
If patients cannot tolerate the nasal CPAP device because of nasal airway obstruction, we proceed with nasal corrective surgery which may include a septoplasty, turbinate reduction with either a laser of radiofrequency device, and correction of nasal valves which become weakened with sleep apnea.
Nasal obstruction typically results in sleep disruption but contributes only a limited amount to sleep apnea. Patients with nasal obstruction and no sleep apnea have worse quality sleep. The purpose of correcting nasal abnormalities is to improve breathing quality at night, and allowing the use of nasal CPAP if patients have sleep apnea.
The other airway levels that obstruct with OSA include the palate which we call the retropalatal (behind the palate) airway, and the retrolingual airspace (airway behind the tongue). The oral appliances improve the retrolingual airway, but do little for the retropalatal airway. The palate contributes about 20% to sleep apnea, whereas, the retrolingual airway is responsible for approximately 80% of sleep apnea. Any surgical procedure must address all of these levels.
Surgery for the palate is very effective for snoring, but is only 50% effective for sleep apnea. This is because most people have retrolingual collapse in addition to retropalatal collapse, so surgery directed at the palate as the sole source of the problem is only partial treatment.
 |
 |
Dr Marc Kerner on Inside EditionDr. Kerner on “Inside Edition” discussing sleep apnea and the signs, symptoms and surgery option |
Procedures for the palate include a uvulopalatopharyngoplasty (UPPP), in which the soft palate is tightened, and tissue is removed to stiffen the palate. If tonsils are present, they are removed at the same time. For people with mild apnea, laser procedures have been used, these typically are quite painful, and do not improve apnea to any significant extent. They are somewhat effective for snoring. There are radiofrequency devices that can be used to shrink the palate tissues and stiffen them at the same time; these sometimes require multiple applications at different times, and are effective for snoring. For patients with large tonsils, and a thick, elongated uvula, radiofrequency procedures are less effective.
When there is evidence of retrolingual collapse (we determine this at the time of the initial examination using a flexible scope to evaluate the entire upper airway) other procedures are indicated to tighten and enlarge the retrolingual airspace. All of the procedures for the base of the tongue either tighten or enlarge this airway.
Radiofrequency devices are used to shrink the tongue; this requires multiple treatments and has been shown to be effective in reducing sleep apnea in a number of clinical trials. A genioglossus advancement is a procedure that we have pioneered that creates a bone muscle flap with the primary muscle of the tongue, and repositions it through an incision in the mouth. This creates a larger airspace and tightens the airway. We usually do this in conjunction with a hyoid-suspension myotomy which is a procedure that enlarges the airway behind the larynx. Multiple procedures can be done at the same time including nasal correction, palate surgery, tongue radiofrequency reduction, and genioglossus advancement/hyoid suspension myotomy.
For patients with skeletal deformities or severe apnea repositioning of the upper and lower jaws are sometimes indicated. This is what we term phase II surgery, and we reserve this for patients who fail phase I surgical procedures, and those with severe craniofacial abnormalities that require skeletal correction. Before these procedures are undertaken, special xrays called cephalometrograms, and panorex films are obtained. Sometimes a CT scan will be obtained for unusual airway findings. Some patients will require orthodonture to reposition the bite in the appropriate location.
When multiple procedures are performed at the same we typically keep the patient overnight in the hospital for monitoring. When the procedures are done individually, they can usually be done on an outpatient basis.
The most important thing to understand is that sleep apnea is a complex disease that requires a proper diagnosis (physical examination and sleep study), and then an individualized treatment plan that begins with conservative therapy (weight loss, sleep positioning, oral devices, and CPAP.) When these treatments are inadequate, or not well tolerated, we then progress to more complex therapies. These include palate surgery, tonsillectomy, either with traditional techniques or with state-of-the-art radiofrequency tissue reduction techniques of the palate and tongue base. Phase 2 surgeries include jaw and tongue repositioning procedures, and craniofacial reconstruction procedures for more severe cases.
Tonsillectomy/adenoidectomy
Tonsillectomy and/or adenoidectomy involves the removal of the tonsils and tonsil-like tissue from the back of the nose called adenoids. The most common cause of obstructive sleep apnea in children is enlarged tonsils and adenoids. The symptoms of obstructive sleep apnea in children include daytime irritability, lack of concentration, and daytime sleepiness. The most common sign is loud snoring, breathing difficulties at night, and nasal obstruction. Most of the time the diagnosis can be made by careful examination, but occasionally the diagnosis is made with an overnight sleep study or polysomnogram.
Tonsillectomy can be performed traditionally by completely removing the entire tonsils. The recovery is 10-14 days and the greatest risk from this surgery is bleeding which typically occurs 7-10 days after surgery. Sometimes this bleeding requires a return to the operating room to control the bleeding. This does not delay the healing process but it does dictate that patients must take it easy with no exercising or strenuous activities for two weeks after surgery. The risk of bleeding is approximately 4-6%.
Radiofrequency Tonsil Reduction
There is a newer treatment option which we have pioneered and utilized almost exclusively over the last 12 years. This entails the shrinkage of the tonsil tissue with radiofrequency energy. This results in significant reduction in the number of infections, a reduction in the size of the tonsil tissue, and has a significant reduction in bleeding risk.
A study presented at the American Academy of Otolaryngology meeting by Dr. Kerner showed the following data:
175 patients with chronic tonsillitis treated with radiofrequency tissue reduction:
94% had complete resolution of symptoms
3 patients needed a simple, retreatment for a rate of 1.7%
Postoperative bleeding rate requiring reoperation—0.6%
Palate surgery
Excessive soft palate tissue is a frequent cause of airway obstruction in obstructive sleep apnea. The most common procedure to treat the soft palate is a uvulopalatopharyngoplasty. Uvulopalatopharyngoplasty is a procedure in which tissue from the palate and/or the back of the throat is removed to increase airway size. However, there are potential significant complications, such as foreign body sensation — a feeling that something is in the back of the throat while swallowing — and velopharyngeal insufficiency — liquids or food escape into the nose while drinking or eating.
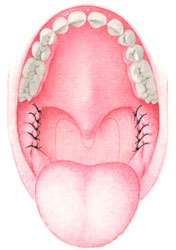
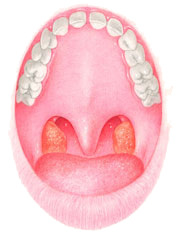
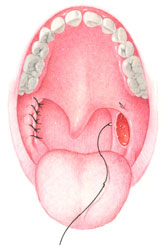
Pharyngoplasty is a significantly less invasive procedure that also achieves improvement of the airway. In this procedure, a minimal amount of tissue is removed as compared to uvulopalatopharyngoplasty or uvolopalatal flap. Tonsillectomy is routinely performed in pharyngoplasty and airway improvement results from tissue rearrangement by suturing the tissue laterally and superiorly.
This procedure is performed in a hospital surgery center under general anesthesia.
This procedure takes approximately one hour. Overnight hospitalization is usually recommended afterward, and in general the patient can usually return to work in 10 to 14 days.
Since minimal tissue is removed during pharyngoplasty, it is associated with less pain and complications than uvulopalatopharyngoplasty or uvulopalatal flap. However, post-operative pain can still be significant, especially when combined with a tonsillectomy. Bleeding represents another potential but uncommon complication.
This procedure is often performed in conjunction with nasal surgery, genioglossus advancement or radiofrequency reduction of the tongue in order to maximize airway improvement.
|
Before Surgery |
During Surgery |
 |
|
Excessive soft palate tissue is a frequent cause of airway obstruction in obstructive sleep apnea. The most common procedure to treat the soft palate is a uvulopalatopharyngoplasty. Uvulopalatopharyngoplasty is a procedure in which tissue from the palate and/or the back of the throat is removed to increase airway size. However, there are potential significant complications associated with uvulopalatopharyngoplasty, such as foreign body sensation — a feeling that something is in the back of the throat while swallowing — and velopharyngeal insufficiency — liquids or food escape into the nose while drinking or eating.
Uvulopalatal flap is a less invasive procedure that also achieves improvement of the airway. In this procedure, a small amount of tissue is removed as compared to uvulopalatopharyngoplasty. Airway improvement results from tissue rearrangement by lifting the soft palate to widen the airway. If the tonsils are still present, a tonsillectomy is always performed with the uvulopalatal flap. This procedure is performed in a hospital surgery center under general anesthesia. This procedure takes approximately one hour. Overnight hospitalization is usually recommended afterward. In general, the patient can usually return to work in 10 to 14 days. Since less tissue is removed in the uvulopalatal flap, it is associated with less pain and fewer complications than uvulopalatopharyngoplasty. However, post-operative pain can still be significant, especially when combined with a tonsillectomy. Bleeding represents another potential but uncommon complication. This procedure is often performed in conjunction with nasal surgery, genioglossus advancement or radiofrequency reduction of the tongue in order to maximize airway improvement.
|
|
|
|
The tongue is a frequent cause of upper airway blockage in obstructive sleep apnea. It can collapse toward the back of the throat during sleep, therefore contributing to obstruction of the airway. The collapsibility of the tongue can be improved with genioglossus advancement. The genioglossus is the primary muscle of the tongue and is attached to a small bony projection on the interior of the lower jaw. During genioglossus advancement surgery this small projection is moved forward and the tongue attachment is repositioned anteriorly so that it is less likely to collapse posteriorly and block the airway during sleep. Dr. Kerner has published articles on this technique (article I wrote)
This procedure is performed in a hospital surgery center under general anesthesia.
This procedure takes approximately 30-45 minutes. Overnight hospitalization is usually recommended afterward and patients usually return to work in 10 to 14 days. While speech and swallowing are not affected, this procedure is typically associated with some pain, swelling and occasional minor numbness of the lower front teeth. This procedure is often performed in conjunction with uvulopalatal flap and radiofrequency reduction of the tongue in order to maximize airway improvement.
The airway is, in essence, confined by the upper and lower jaws. By moving the upper jaw (maxilla) and lower jaw (mandible) forward, the entire airway can be enlarged. This procedure serves as the most effective surgical treatment for obstructive sleep apnea. It is performed on patients with moderate to severe obstructive sleep apnea as the only treatment, or when other procedures have failed. It is also performed in patients with significant jaw deformity that contributes to obstructive sleep apnea.
This procedure is performed in a hospital surgery center under general anesthesia.
Maxillomandibular advancement surgery is three to four hours in duration. Hospitalization is usually two to three days and in general the patient can return to work in four weeks.
In general, the jaws do not need to be wired after surgery as they are stabilized. The integrity of the bite is preserved through the use of small titanium plates and screws, as well as braces (or arch bars) and rubber bands. Chewing is avoided for four weeks. Speech and swallowing are not affected but this procedure is associated with pain, swelling and temporary numbness of the lower lip and chin. Some changes in facial appearance will occur but is usually quite acceptable. This procedure is occasionally performed with genioglossus advancement or nasal surgery.
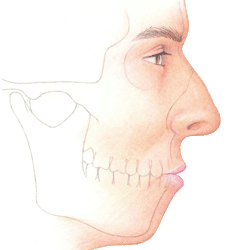 Before Surgery Before Surgery |
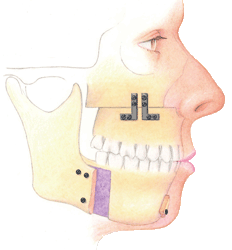 After Surgery After Surgery |
Indications for sleep surgery
- Excessive Daytime Sleepiness ( Altered daytime performance )
- RDI >20*
- Oxygen saturation < 90%
- Arrhythmias ( cardiovascular derangements )
- Negative Pes ( esophageal pressure ), more negative than -10 cm H20 during sleep
- Treatment for an RDI < 20 acceptable in cases where excessive daytime sleepiness (EDS) causes altered daytime performance (mild OSAS and UARS)
Current Methods of Management:
Medical:
- CPAP/BIPAP *
- Weight loss
- Sleep hygiene
- Dental splints or tongue retaining devices
Surgical:
|
Pre-surgical evaluation:
Prior to any surgical procedure, a patient will need to be evaluated. This evaluation will typically include:
- Polysomnography
- A comprehensive history
- Head and neck physical examination
- Fiber-optic nasopharyngoscopy-sleep endoscopy
- Lateral cephalometric analysis
This evaluation will give sufficient information to help in directing surgical therapy and in addressing the possibilities for treatment or clinical outcomes. This systematic medical and surgical review will support the establishment of the following guidelines:
- Determine sleep disorder type
- Establish parameters of severity
- Identify co-morbidity factors
- Identify probable sites of obstruction
- Decide if treatment is emergent or elective
- Assess the risk/benefit ratios
Classification of Obstructive Region by S. Fujita
- Type l Palate (normal tongue base)
- Type ll Palate and base of tongue
- Type lll Base of tongue (normal palate)
Oropharyngeal Obstruction: Reconstruction
Rationale: The palatal and lateral pharyngeal tissues have been found to be the most compliant of the upper airway; documentation of the collapse at this level in SDB is well established.
Indication:
- A long soft palate
- Narrow inlet to the nasopharynx
- Hypertrophic tonsils
- Redundant lateral pharyngeal mucosa. This level of obstruction is classified as a Fujita Type 1
Techniques: There are multiple methods to control this region and range from the traditional UPPP to the Uvulopalatal flap procedure. There many variations of the original procedure. Lasers, cautery or radiofrequency technologies have been employed to perform this surgery.
Clinical outcomes: Individual results vary with the skill of the surgeon and the technique selected. The technique has not gained widespread popularity over the years due to the pain and discomfort after surgery and the varied cure rate. Many UPPP’s did clear the pharyngeal level of obstruction and were unfairly credited with failure due to the unrecognized tongue base problem (hyopharyngeal). In patients who have been carefully selected for upper airway reconstruction and whose site of primary obstruction is at the oropharyngeal level (Fujita type 1), the cure rate may be 80 to 90 %. In unselected patients this rate will fall to a low of 5 to 30%.
Hypoharyngeal Obstruction: Reconstruction
Rationale: Tongue base obstruction has been documented in SDB by EMG studies, fiber-optic exams, radiographic cephalograms, CT and MRI scans and vidiofluoroscopy. In addition, the basic anatomy and physiology of the skeletal relationships have led to a better understanding of how to surgically approach the base of tongue level.
The obstruction of the hyopharyngeal (base of tongue) region is a very complex problem. This region may be bypassed by tracheotomy or approached logically by either making more room for the tongue or reducing the tongue size. This procedure is referred to as part of Phase One of the sleep surgery protocol. This is a simple technique that does not move the teeth or jaw and does not interfere with the dental bite. A more aggressive procedure, usually saved for failure of the more conservative surgery above, is the forward movement of the lower jaw and midface (maxillomandibular advancement surgery). This procedure is referred to as Phase Two of the Powell-Riley phased protocol. This gives the tongue more room, also placing additional tension on the tongue base.
A tracheotomy is the most extreme surgical procedure but is the most effective since it completely bypasses the obstructive region. It is generally used in patients where other procedures have failed. Many patients cannot accept this as a solution unless they are morbidly obese, or cannot use CPAP.
The most conservative treatment is offered as an entry-level procedure by our surgeons. We have named this approach to upper airway reconstruction “multilevel airway reconstruction,” and over the years it has proven to be an effective and safe method for controlling upper airway collapse in sleep-disordered breathing. It has additionally reduced the possibility that unnecessary surgery would be performed.
Definition of Responder or Cure: (Powell-Riley) Criteria must include 1-4 below or items 4 and 5 are completed.
- RDI < 20 and /or at least a reduction in the RDI of 50% only if the initial RDI was less than 20 (for example if the RDI is 25 then it must be 12.5 after treatment to call it a cure)
- Sa02 > 90% or a minimal fall below 90%
- Normalization of sleep architecture
- Resolution of excessive daytime sleepiness (EDS)
- Equivalent comparison to nasal CPAP/BiPAP results on a full night titration
Three regions of the upper airway are treated as directed by the clinical work-up, primarily the sleep endoscopy, which gives us the most useful information for which surgical procedures to perform. We utilize the most conservative surgery for each, but only including treatment at that level if it was considered sufficiently obstructed.
All nasal abnormalities are corrected. This depends on the type of anatomic deformity (septum, turbinates, sinus obstruction, or nasal valve deformities). We typically perform nasal surgery first as a separate procedure. Once healed, we then address the other airway levels. A UPPP or equivalent and tonsillectomy is performed if tonsils are present. For addressing the tongue region we then proceed to genioglossus advancement, hyoid myotomy and suspension, or laser midline glossectomy and lingualplasty, or partial glossectomy.
After Phase One is complete, a period of 4-6 months is allowed for sufficient healing, weight stabilization and neurologic equilibration. Then a repeat polysomnogram accompanied with a sleep assessment and clinical examination is done to assess the clinical outcomes. Those patients who are unchanged or incompletely treated are offered either further surgery consisting of maxillomandibular advancement surgery, tongue base reduction, tracheotomy or nasal CPAP.
|
Our philosophy is of treatment is as follows: Treat to cure, logically direct treatment to specific anatomic regions, full disclosure of options and risks of surgery versus no surgery, staged surgical management, and follow-up of all treatments.
For further information contact us at (818) 349-0600.





 During Surgery
During Surgery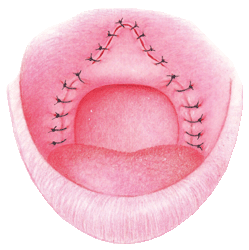 After Surgery
After Surgery Dr Kerner on KFWB discussing Sleep Deprivation
Dr Kerner on KFWB discussing Sleep Deprivation