Voice and Swallowing Center
Voice Disorders and Laryngology
 Patients with hoarseness, loss of voice, difficulty singing or speaking are evaluated at either office. We are equipped with state-of-the-art voice laboratories at all of our offices. The key to the successful management of voice disorders requires a precise diagnosis. The study of the larynx (called laryngology) is in its infancy. We are just now beginning to understand the complex relationships of the larynx (voice box) to a number of related conditions such as reflux disease. To properly treat patients with the symptoms of hoarseness, voice change, difficulty singing, or voice weakness, we require a detailed, comprehensive evaluation that begins with our voice questionnaire. This can be downloaded for your use prior to our evaluation.
Patients with hoarseness, loss of voice, difficulty singing or speaking are evaluated at either office. We are equipped with state-of-the-art voice laboratories at all of our offices. The key to the successful management of voice disorders requires a precise diagnosis. The study of the larynx (called laryngology) is in its infancy. We are just now beginning to understand the complex relationships of the larynx (voice box) to a number of related conditions such as reflux disease. To properly treat patients with the symptoms of hoarseness, voice change, difficulty singing, or voice weakness, we require a detailed, comprehensive evaluation that begins with our voice questionnaire. This can be downloaded for your use prior to our evaluation.
Dr. Kerner reviews the detailed history prior to an examination. We utilize specialized diagnostic equipment in our voice laboratory. The examination consists of a complete head and neck examination, a vocal capability battery if indicated and a videostroboscopy. The key to successful treatment outcomes is a precise diagnosis. We cannot accurately reach the appropriate diagnosis without a complete evaluation.
Videostroboscopy
We specialize in treating patients that have difficult to diagnose voice problems, voice weakness, and vocal cord paralysis, and professional voice users such as singers, actors, performers, teachers and attorneys.
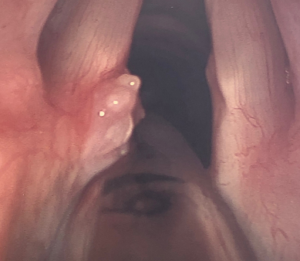
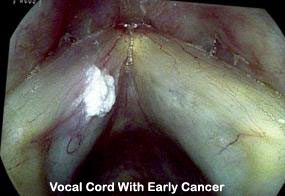
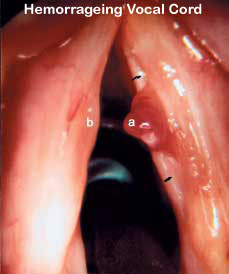
These are images of various vocal cord problems:


Vocal Cord With Cyst

Many people get vocal cord lesions:


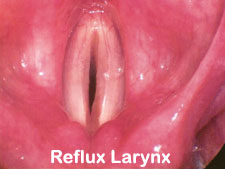
Treatment Options
 Most patients are successfully treated with a combination of medical therapy consisting of voice and/or speech therapy, in addition to medications for underlying medical problems. We work closely with speech therapists, voice coaches, and other voice specialists to assist in the rehabilitation process. In many cases, this type of therapy is far more important than surgery. Of course, all treatment plans are devised on an individual basis. Reflux is by far and away the number one cause of vocal problems in most patients. It is a contributor to vocal cord lesions, hoarseness and a myriad of voice disorders.
Most patients are successfully treated with a combination of medical therapy consisting of voice and/or speech therapy, in addition to medications for underlying medical problems. We work closely with speech therapists, voice coaches, and other voice specialists to assist in the rehabilitation process. In many cases, this type of therapy is far more important than surgery. Of course, all treatment plans are devised on an individual basis. Reflux is by far and away the number one cause of vocal problems in most patients. It is a contributor to vocal cord lesions, hoarseness and a myriad of voice disorders.
Patients with surgical problems such as suspicious lesions on the vocal cords, cysts, masses, or paralysis can be readily treated with microsurgical techniques. Our surgical techniques utilize microscopic cold knife surgery of the vocal cords termed “phonomicrosurgery.” Patients undergo this type of procedure as outpatients, and are discharged within a few hours of the procedure. For patients with papillomas Dr. Kerner utilizes state-of-the-art instrumentation to perform microlaryngeal phonosurgery.
 This is an example of a right vocal fold lesion which is a benign cyst. The patient is a professional singer and this was severely affecting her ability to perform. She was misdiagnosed multiple times as having a singer’s nodule which did not get better with voice rest.
This is an example of a right vocal fold lesion which is a benign cyst. The patient is a professional singer and this was severely affecting her ability to perform. She was misdiagnosed multiple times as having a singer’s nodule which did not get better with voice rest.
 This is the view of the vocal fold after microscopic removal of the cyst and lesion. After a short recovery period, she has returned to successfully singing, performing and recording music.
This is the view of the vocal fold after microscopic removal of the cyst and lesion. After a short recovery period, she has returned to successfully singing, performing and recording music.
The postoperative care varies depending on the exact surgery performed, but in general, most patients are put through a three-part rehabilitation regimen following surgery.The first phase of the recovery and rehabilitation involves complete voice rest for 48-72 hours. This depends on the type of surgery performed and the extent of healing required. The second phase of the rehabilitation process begins after 10 to 14 days after surgery. This involves gradual reintroduction of voice use with absolute avoidance of behaviors such as yelling, talking on the telephone, or lecturing.
In this second phase, voice therapy is introduced, and a vocal hygiene program is initiated that involves behavior modification, medical therapy and close follow-up. Phase 3 of the rehabilitation process begins approximately 12 weeks (3 months) after surgery.
Voice Disorders
Laryngology is the study of the larynx, or voice box. It is an area that has become increasingly complex as we learn more about the voice.
People who study Laryngology fall into one of a few categories:
Physician: physicians such as Dr. Kerner who study Laryngology have completed the training and have extensive experience in the treatment of laryngeal and voice disorders.
Comprehensive care of the professional voice
There are a number of occupations that require significant voice use including teaching, singing, acting, sales and others who talk for a living. Recreational activities can also be vocally demanding, such as coaching. Any profession that requires three or more hours of speaking or singing per day is considered to be vocally demanding. Increased voice stress occurs when working in noisy environments such as construction sites, factories, or classrooms. Speaking or singing for greater than one hour at a time is also considered to be stressful on the voice. Even highly trained voice users (e.g., professional singers, actors) can develop voice problems, despite good vocal technique.
Hoarseness is roughness or an undesirable voice quality, vocal fatigue (voice wears out or worsens with use), fluctuating voice quality, reduced volume or pitch flexibility, and pain or soreness associated with voice use. Any sudden or severe voice changes should be evaluated immediately as should the gradual onset of hoarseness, vocal fatigue, or other symptoms of laryngitis that persist for longer than three weeks should be evaluated as well.
What is a Voice Problem?
The American Speech, Language and Hearing Association defines a voice problem as having a pitch, loudness or vocal quality which draws attention to itself rather than to what the speaker is saying. A voice problem may also include pain, discomfort or fatigue when voicing. Voice Disorders range from a mild laryngitis to severe life-threatening diseases that may require extensive treatments. Any hoarseness or voice change which persists for longer than two weeks should be medically evaluated.
Some common signs of a voice disorder include:
Hoarseness
Loss of voice, voice breaks
Changes in pitch
Shortness of breath while speaking or singing
Difficulty maintain/initiating soft voice
Difficulty maintain/initiating loud voice
Sore or scratchy throat
Vocal fatigue when talking
Neck and/or jaw muscle tension
Loss of singing range
Prolonged warm-up time
Constant throat-clearing or coughing
Dry throat or mouth
Tickling or choking sensation
Difficulty swallowing
Lump in throat
Frequent bad breath
Excess mucous or phlegm
Acidic taste in mouth
Calwest Voice and Swallowing center consists of specialists who will offer a thorough functional and objective diagnosis followed by treatment plans using state of the art equipment and an extensive network of consultants.
Bowed Vocal Chords
Bowed Vocal Folds is a term used to describe vocal folds that have lost muscle bulk due to injury, aging or neuromuscular diseases. Bowed vocal folds fail to come together and then result is usually a breathy voice sound and effortful phonation.
Chronic Cough
Chronic Cough is a cough lasting more than 2 months that does not resolve with rest or medication. A chronic cough usually has multiple causes. Treatment requires pharmacological intervention and behavioral management.
A program of respiratory retraining is a specialized treatment that is used to resolve chronic cough when it is associated with abnormal movements of the vocal folds known as paradoxical vocal fold motion disease (PVFMD).
Chronic Cough is a common problem seen by Dr. Kerner and Associates. It is often treated without success as a sinus, allergy or lung problem or as a functional problem that people are told to “live with it.” Chronic cough can be extremely debilitating. One of the most often overlooked causes of chronic cough is Paradoxical Vocal Fold Motion Disorder (PVFMD). PVFMD is known by many different names such as vocal fold dysfunction, vocal stridor, irritable larynx syndrome and adult onset asthma.
Symptoms of PVFMD
Patients with PVFMD complain of severe long-term cough, occasional changes in voice quality, increased breathing difficulty around soap powders, perfumes and other odors, shortness of breath or air hunger and even wheezing or other breathing noises associated with breathing. Despite the use of steroids, inhalers or other pharmacological agents, the cough and breathing difficulties persist in people with PVFMD.
Diagnosis
At Calwest Voice and Swallowing Center, a standard series of tests are used to diagnose PVFMD. The first part of any examination is a thorough case history relating to the onset, severity and previous treatments of the problem. Next is a videostroboscopic examination of the larynx and vocal folds. In this exam, the patient is given specific vocal and breathing tasks to perform while the larynx and vocal folds and the entire exam is recorded on DVD in order to study the motions during each of the tasks. The video exam of the larynx is followed by a breathing test to identify the breathing components related to the lungs and the upper airway.
Treatment
Treatment for PVFMD is comprehensive and is often accompanied by laryngopharyngeal reflux (reflux sheet) an inflammation of the larynx caused by stomach acid in the larynx. Proper medication is the first step in the treatment. This is followed by a series of breathing exercises known as respiratory retraining. Respiratory Retraining focuses on coordinating breathing with vocalization. This technique has been shown to be useful for patients with excessive cough, paradoxical vocal fold motion disorder, vocal spasm or laryngeal irritation. It is used in conjunction with the treatment of laryngopharyngeal reflux. The exercises consist of rhythmic breathing using minimal inhalation effort and working up to active exercises combining breathing and vocalization in specific rhythmic patterns. Treatment of PVFMD may take as little as 3 weeks or as much as 6 months. The treatment is highly successful and results in a vastly improved quality of life for those who have suffered with cough.
What is Hoarseness?
Hoarseness is a common term used by most people to describe changes in the voice that make it sound abnormal. When a voice is not normal, it is said to be “hoarse”. Actually, there are many types of hoarseness or voice quality changes that if left untreated will limit one’s ability to communicate effectively, cause a loss of income or lead to serious medical conditions. Hoarseness (the technical term is dysphonia) has many causes and is only a sign that a problem exists with the vocal folds, the muscular structures that vibrate to produce sound for speech and singing.
How is the voice produced?
The vocal folds (vocal cords) are housed inside the larynx, the structure in the neck easily identified by the prominent “Adam’s apple.” The vocal folds lie right behind the Adam’s apple. The vocal folds produce sound when they come together and are driven by the air supply from the lungs. In order for sound to be clear and not hoarse, the vocal folds must move together symmetrically, be capable of opening and closing regularly and then have sufficient air flow from the lungs to keep them vibrating. The vocal folds are capable of vibrating at speeds as low as 10 times a second all the way to 1200 times a second, as in a soprano singing a high note. However, when the voice is hoarse, the vocal folds may fail to close, fail to vibrate symmetrically or fail to maintain vibration at a steady rate.
How are voice problems diagnosed?
A comprehensive evaluation of hoarseness includes a detailed history or voice usasge and an examination of the larynx and the vocal folds. The details surrounding the onset of the problem are particularly important. How, when, where and under what conditions did the problem begin? The evaluation of hoarseness includes a perceptual assessment of voice quality – pitch, loudness, pitch breaks or other changes from the normal voice. Instrumental assessment of the voice including measurement of pitch and loudness range, and clarity (called perturbation) is an important part of the evaluation.
How are the vocal folds examined?
Visual examination of the vocal folds is the key to a comprehensive evaluation of hoarseness. The examination of the vocal folds may be done with a rigid endoscope that shines a light onto the vocal folds from the mouth. Video strobolaryngoscopy is a special examination technique that uses a special light and microphone to synchronize the movements of the vocal folds so they may be viewed in slow motion. The details of vibration and vocal fold motion are recorded for review and permanent record. Examinations are routinely conducted in the office and take only a few minutes.
Treatments of hoarseness may include medications, voice therapy, surgery or all of these. Voice therapy is a behavioral technique that consists of vocal hygiene, a daily plan for avoiding voice misuse, strain and over use, Voice therapy also consists of vocal exercises, respiratory support management and vocal relaxation. Voice therapy is used to return the voice to its highest and best use after injury or surgery. Voice therapy is the treatment of choice for many voice disorders. Voice therapy is conducted by a certified and licensed speech-language pathologist after vocal fold examination. Comprehensive care of hoarseness may also require surgery if changes are not responsive to voice therapy or medications.
Hoarseness which lasts for two weeks or more requires a comprehensive diagnosis and treatment to prevent further injury or damage to the voice and return the voice to normal use.
Laryngeal Papilloma
Laryngeal Papilloma are growths on the larynx thought to be caused by a viral infection.
Muscle Tension Dysphonia
Muscle Tension Dysphonia is a voice disorder characterized by strained, effortful phonation usually causing vocal fatigue if used extensively.
Two types are known:
Primary muscle tension dysphonia – a type of vocalizing or speaking in which the muscles in the neck are tense and when no other lesion or paralysis is seen.
Secondary muscle tension dysphonia – a compensatory method of vocalizing due either to a paralysis, paresis or muscular weakness causing the person to squeeze other parts of the larynx to help produce sound.
Reflux
Reflux refers to the backflow of stomach contents into the esophagus and/or throat.
Reflux Laryngitis
Reflux Laryngitis is hoarseness and voice change due to reflux material coming up to the level of the larynx.
Reinke’s Edema
Reinke’s Edema is swelling of the vocal folds due to trauma or noxious irritations (cigarette smoking) resulting in a deeep husky voice. Women with Reinke’s Edema are often mistaken for men on the telephone.
Singer, Actor and other Voice Professional Voice Problems
Singers, actors and other voice professionals require special care of their voices. Every singer and actor has a unique vocal signature that he or she must maintain despite injury or sickness.
At Calwest Voice and Swallowing Center we offer comprehensive, conservative management of voice disorders of the singer and actor. Like other professionals, singers and actors may injure their voice from time to time due to excessive use, new repertoire or performance in less than ideal surroundings. The performer should seek early care to avoid problems.
The voice professional should follow a few simple rules in order to keep the voice healthy:
– Warm up before singing or performing
– Don’t perform when sick
– Know your role well
– Rest before and after performances
– Know when to stop talking or singing
– Get help sooner than later
– Beware of performance enhancers (drugs and alternative medicines)
Injuries to the voice can occur at any time. Upper respiratory infections (URI) and common colds are two problems that affect the way a performer may develop voice problems. Singing or speaking with poor acoustics or in unhealthy environments may also lead to injuries.
Two kinds of injuries often seen in the Voice & Swallowing Center are vocal fold edema (swelling of the vocal folds) and vocal fold hemorrhages. Both require conservative treatment. Voice rest, and medications to treat the upper respiratory infection usually restore the voice to its normal use. Continued singing or performing once a problem is noted may lead to serious injuries that threaten a career.
Some singers and performers are concerned that they developed a voice problem because they are using their voice incorrectly and therefore may not be truly professional. This philosophy is not correct and may lead to avoidance of treatment. Vocal performers should be considered to have long careers and like other professional athletes may develop problems from time to time that restrict their performance.
Successful care and treatment of the professional is now available. Performers should take advantage of the high level of voice care available at Calwest in order to preserve their careers and enhance their level of performance.
Spasmodic Dysphonia
Spasmodic Dysphonia is a disabling disorder of the voice characterized primarily by involuntary disruptions of phonation. It may also be accompanied by hoarseness, tremor, and pitch breaks. This disorder was originally thought to be psychological in origin. However, in recent years, spasmodic dysphonia has become classified as a movement disorder of the larynx. Thus, spasmodic dysphonia is a vocal dystonia. There are two general types of spasmodic dysphonia. Adductor spasmodic dysphonia (ADSD) is characterized by a squeezed, strained-strangled effortful phonation with voice stoppages and voice breaks. Abductor spasmodic dysphonia (ABSD) is characterized by an excess flow of air with intermittent lack of vocal fold closure. In some cases, patients have evidence of of both types. By far, the most common of these is the adductor type. In ADSD, irregular spasmodic movements of the vocal folds and hyperadduction of other structures in the larynx severely affect the ability to communicate.
Botox has since become the choice of treatment for patients with spasmodic dysphonia. For ADSD, botox is injected into the thyroarytenoid muscle by passing the needle between the cricoid and thyroid cartilages and into the vocal fold. For ABSD, the posterior cricoarytenoid muscle is usually injected. Although dosages and injection techniques vary, botox has become the choice of most patients and physicians for treating spasmodic dysphonia. Botox injection leads to symptom relief for up to six months and occasionally longer with few or no long term effects. Patients report less effort to vocalize one or two days after treatment. Although the treatment is temporary, the effects of botox are significant from a communication standpoint. That is, patients are able to engage in social conversation without the stigma of voice breaks and voice stoppages.
Treatment of spasmodic dysphonia begins with an accurate diagnosis. The diagnostic work up generally consists of a thorough case history, including neurological history. Although most patients have some difficulty in pinpointing the exact onset of the disorder, they generally describe a slow, progressing form of voice difficulty that consists of voice breaks, some degree of hoarseness, more difficulty speaking in noisy situations, and increased difficulty when attempting to use a loud voice. Acoustic and aerodynamic assessments of the voice are made to determine the severity as well as to objectively identify the presence of voice breaks. A flexible endoscopic examination of the larynx and vocal folds is also conducted. Videolaryngoscopic examination is necessary to rule out other diseases and conditions that may sound like spasmodic dysphonia. These include vocal fold atrophy, vocal fold paralysis, muscular tension disorders, and the presence of lesions on the vocal folds. If the patient does not have a current neurological examination, the patient is referred to a neurologist for comprehensive evaluation.
Following the evaluation, patients are given a thorough explanation of spasmodic dysphonia. Patients are advised that although other treatments are available, botox injection is the current choice of treatment at this point for this disorder. The patient returns for botox injection after he or she has had a chance to consider the alternatives, be examined by a neurologist, and discuss the treatment options with his or her family physician. Treatment consists of injections generally to both thyroarytenoid muscles. After applying a local anesthetic to the neck area and attaching electrodes to the patient to monitor needle placement, a small needle is inserted between the thyroid and cricoid cartilages and directed up to the vocal fold. In most cases of adductor spasmodic dysphonia, botox is injected into each thyroarytenoid muscle. In patients with severe ADSD, dosage may be greater, up to 2.5 units in each muscle. For those patients with ABSD, approximately 1.25 units of botox is injected into the posterior cricoarytenoid muscle on each side. This muscle has been found to be somewhat more difficult to reach. Thus, there has been less success with treating abductor spasmodic dysphonia in this way. In some cases, the dosage may be greater on one side if upon examination there was evidence of greater spasm activity on one side. The entire treatment process takes about 15 minutes and the patient is free to leave after the treatment.
Three to five days after treatment, the patients report back by telephone the changes in voice and other side effects such as possible swallowing difficulties in the ADSD group or breathing difficulty in the ABSD group. For patients with ADSD, the voice usually changes to a breathy quality 24 to 48 hours after injection; difficulty in swallowing liquids may occur because the vocal folds are weakened by the injection. For patients with ABSD, the side effects may be shortness of breath or difficulty breathing when doing exercise. If the conditions last longer than a week, a note of it is made and injection is slightly reduced in follow up treatments.
Approximately 10 days after injection, patients are invited to return for voice therapy. Voice therapy coupled with botox injections has been shown to extend the effects of injection as well as to give the patient a feeling of control over his or her voice. In our clinic, voice therapy begins approximately 10 days to two weeks after botox injection. Approximately six sessions of treatment are planned, and these are spread over a four to five week period. Voice therapy is an option, however, it is highly encouraged to treat the maladaptive compensatory strategies developed prior to botox treatment. The goal of voice therapy in the ADSD patient is to reduce hyperclosure of the vocal folds, to improve voice onset and to control breath flow over the length of a phrase. In patients with ABSD, easy onset followed by reduced explosion of sounds is the focus. By the final session, patients are encouraged to use the practice exercises they are given and to follow up with additional voice therapy. By monitoring the injection during the first four to five day we get a sense of the accuracy of the injection, the strength of response and the quality of the voice. From this information the dosage on the next treatment can be adjusted if necessary. With the addition of voice therapy after botox injection, the patients will extend the time between treatments by as much as 12 to 15 weeks. This is especially true in the ADSD subjects.
The treatment of spasmodic dysphonia continues to be investigated by numerous scientists studying movement disorders. New treatments are needed since botox is not a cure but a temporary relief. Surgical treatments that have been used in the past have also shown success as a treatment but not necessarily a cure. Current investigations include new surgical procedures to treat the disorder, other medications that may help to control movement disorders and improve management of the patient after botox injection. When one considers the significant debilitation caused by spasmodic dysphonia, whether it is ADSD or ABSD, treatments that provide relief are most welcome to all patients.
Vocal Fold Atrophy
Vocal Fold Atrophy is loss of muscle bulk in one of the voice muscles.
Vocal Fold Cysts
Vocal Fold Cysts are benign lesions on the vocal folds that may either be filled with mucous (mucous retention cyst) or a fibrous mass on the vocal folds.
Occasionally, the cysts reside deep in the tissue of the vocal fold and causes the vibratory pattern to be restricted in motion. In children and some adults, cysts may have a contralateral mass lesion and it may be difficult to determine if these are cysts or vocal nodules.
Video laryngostroboscopy is necessary to properly diagnose these lesions.
Vocal Fold Granuloma
Vocal Fold Granuloma is an area of thickened, irregular tissue on the vocal fold caused by irritation.
Vocal Fold Paralysis
Vocal Fold Paralysis is damage to the recurrent laryngeal nerve or superior
laryngeal nerve that can produce a vocal fold paralysis. These are branches of the X Cranial Nerve. When the vocal fold is paralyzed, it loses its mobility.
Voice Misuse
Excessive shouting, screaming or throat clearing are all behaviors that contribute to voice misuse and possibly to an injury to the voice.
Other things such as throat clearing, breathing noxious fumes (second hand smoke), cigarette smoking, excessive use of alcohol, use of street drugs and attempting to speak or sing while sick or under excess stress are all part of vocal misuse.
Vocal Nodules
Vocal Nodules are bilateral symmetric lesions on the vocal folds that develop from excessive and improper use of the voice. They occur mostly in young boys and in adult females. These lesions are similar to callouses on the hands or feet.
Vocal nodules are treated with voice therapy and vocal hygiene and usually go away when the vocal abuse or misuse is eliminated.
Vocal Papilloma
Papillomas are benign epithelial tumors that are caused by infection with the human papilloma virus (HPV). They are the most common benign neoplasms affecting the larynx and upper respiratory tract.
Although papillomas are benign, their rapid growth can cause obstruction of the airway that can lead to asphyxiation if not treated.The papilloma can affect the vocal folds and/or epiglottis, and can occasionally spread distally to involve the trachea or bronchi.
Vocal Polyps
Vocal Polyps are benign epithelial lesions of the vocal folds that are fluid filled and usually unilateral. The fluid filled area usually causes asymmetry in the vibration of the vocal folds.This often results in a wet hoarse quality of the voice.
Vocal polyps are treated with surgery after vocal hygiene and voice therapy.
Dr Marc Kerner on CBS2 News
Dr. Marc Kerner on CBS2 News discussing survival rates for throat cancer surgery.
==========================
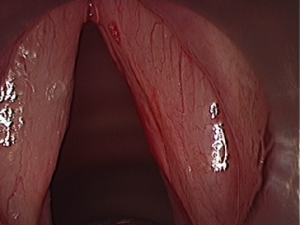
Before and after of a left vocal cord mass-removed microscopically first pic shows the mass on the left side, the next one is just after removal and the third is the mass